Blog
Our latest news and thoughts
- All Posts
-
- Healthcare
- Remote Patient Monitoring
- Connected Care
- Patient Satisfaction
- Digital Innovation
- Standard of Care
- CMS
- Connected Health Devices
- Medicare
- Reducing Expenses
- Connected Health
- Patient Provider Relationship
- Bundled Payments
- Bundled Payments for Care Improvement
- Clinical Empathy
- Coronavirus
- Entrepreneurship
- Optimize Costs
- Physician Burnout
- Revenue
Remote Patient Monitoring & Connected Health: A New Standard of Care
Topics: Remote Patient Monitoring, Patient Satisfaction, Standard of Care
November 19, 2019
by John O'Connor
The Center for Medicare & Medicaid Services (CMS) is serious about using tech to improve healthcare quality. With their sights set on Chronic Care Management (CCM) and Remote Patient Monitoring (RPM), we can expect a new standard of care.
CMS is betting on RPM to catch problems sooner, better connect providers and patients, and improve health outcomes.
While CMS has had codesets for CCM and RPM activities for some time, last year these services finally became eligible for reimbursement. In January of 2019, CMS added three RPM codes to the Physician Fee Schedule, further demonstrating their support for the use of technology-based tools to decrease costs, increase healthcare access, and improve the quality of services delivered.
It’s not just CMS who believes in RPM. In 2017, the FDA released the Digital Health Innovation Action Plan which details a new regulatory framework for digital health software and provides guidance for product developers navigating the medical device industry. Think tanks and thought leaders are also weighing in. A study by the eHealth Institute, for example, reveals that “hospitals and health systems are finding better value in health data collected from the home than they are in traditional office or hospital visits”.
Easy, consistent collection of patient data gives a more complete picture of an individual’s total health, allowing physicians to act on insights to provide highly personalized care.
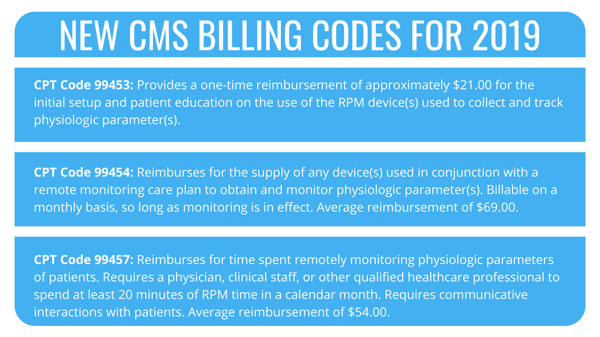
Those who are familiar with CMS’ previous iterations of RPM codes likely see some similarities. Differentiating the 2019 code 99457 from the 2018 code 99091 is the eligibility of clinical staff (medical assistants, RNs, etc.) to assist in RPM services. So, what tools are needed to cash in on RPM?
Incorporating Connected Health and Remote Patient Monitoring in my Practice
Connected Health models utilize digital health tools that allow providers to engage in RPM. Knowing that each practice is unique, providers are able to choose the best-suited technology for their needs. There are many ways to utilize Connected Health in your practice. Here are some of the latest:
- Automated Patient Reminders/Notifications
- Wearable Health Devices
- Virtual Visits
- Mobile Health (mHealth) Applications
- PatientOne
As costs continue to skyrocket and patients’ expectations of digital “health-on-demand” increase, electronic tools providing connected care are no longer items of luxury, but a necessity. Not all Connected Health solutions are created equal, however.
As an early entry into the RPM space, PatientOne can provide the Connected Health tools, reporting, and verification of services to ensure successful RPM programs. PatientOne has developed a solution that provides opportunities for physicians to get paid for services that have typically been done without compensation, provides outstanding care for their patients, and improves efficiency.
While the healthcare industry has been slow to adopt wearables and remote monitoring technology, the tide is turning. Next-generation devices and cloud-based applications are key for quality improvement in healthcare services and processes, and patients love it. Case studies at our beta site even reveal over 90% patient satisfaction and nearly 96% of patients believe that PatientOne was instrumental in receiving better care.
PatientOne allows care teams to intervene quickly, keep patients on track, and catch issues before they become problems. Though this type of care delivery model likely differs from yours, the momentum behind Connected Health will only continue growing.
Sources: CMS, Kaiser Foundation, eHealth Institute, The National Law Review
 John O'Connor is the COO of Patient One and the Practice Administrator at Five Valley's Urology. John co-founded Patient One in 2016 and brings over 25 years of medical administration experience with a proven track-record of solving complex problems. John is passionate about using technology and innovation to eliminate inefficiency and waste radically improve the quality of care in the healthcare field.
John O'Connor is the COO of Patient One and the Practice Administrator at Five Valley's Urology. John co-founded Patient One in 2016 and brings over 25 years of medical administration experience with a proven track-record of solving complex problems. John is passionate about using technology and innovation to eliminate inefficiency and waste radically improve the quality of care in the healthcare field.